Introduction
Patellar tendinopathy (also known as jumper's knee) is a disorder of the patellar tendon that includes tendinosis (characterised by a degenerative disease of the tendon as the main underlying causal mechanism) and tendonitis (characterized by inflammation of the tendon) - the latter being regarded as a wrongly used term applied to this disease condition(1). The disorder manifests as well circumscribed pain at the lower pole of the patella and in the anterior zone of the knee(1). The pain is insidious at first and is triggered by physical activity. However, pain gradually becomes more persistent as the frequency and intensity of exercise increase(2).
Patellar tendinopathy accounts for 30-45% of all lesions experienced by jumping athletes(3,4,5,6). The disorder has a strong sports impact, with worrisome data such as those reported by Lian et al.(3), who found that one-third of all athletes requiring treatment because of patellar tendinopathy are unable to return to their sports activity for at least 6 months. It can also affect the occupational activity of non-athletes, with a prevalence of 8-50%, depending on the type of job activity(4). Because of this, it is important to consider that there might be a lack of awareness during diagnostic evaluation, which may prove insufficient and can probably lead to failure of conservative and surgical treatment. In order to define the disorder and describe the most common clinical and therapeutic factors, the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA) published a consensus document(5,6) based on the best available clinical evidence, and in the same way as in the present study, the document included articles with a scientific level of evidence III-IV.
The present study comprises a literature review focused on the clinical and imaging diagnosis and the different classifications and functional assessment scales, with a view to presenting the patellar tendinopathy diagnostic evaluation and classification recommendations of the Muscle and Tendon Injuries Working Group (Grupo de Estudio de Lesiones Músculo Tendinosas [GELMUT]) of the Spanish Association of Arthroscopy (Asociación Española de Artroscopia [AEA]).
Medical history and examination
The diagnosis is essentially clinical and is generally based on the medical history and the findings of the physical examination. Correlation between the imaging test data and the clinical evaluation corroborates and guides the diagnosis and the patient recovery process. Patients usually report pain in response to palpation of the deep part of the tendon at the point of its insertion in the lower pole of the patella. The pain is of an insidious nature and generally manifests on starting sports activity. It is important to ask about when the pain starts, since it is a determinant factor in one of the classifications (described further below). Exploration in supine decubitus should be performed with the knee in full extension and the quadriceps femoris muscle relaxed. Positioning the knee in 90º of flexion would increase tension in the tendon, thereby lessening its sensitivity(1). In their systematic review, Morgan et al.(7) underscore that in the physical examination it is important to perform a pain provocation test (single-leg squat test) involving a single-leg squat with the knee in 30° of flexion and the other knee extended (Figure 1), as described by Malliaras et al.(8). This test produces considerable tension in the patellar tendon that in turn causes pain in the presence of tendinopathy. According to Malliaras et al.(8), the load tolerance principle is the most important part of patellar tendinopathy rehabilitation, and is useful for quantifying the results of treatment. Lastly, it is useful to point out that quadriceps atrophy and hypotonia are common findings, and that sudden and rapid contraction of the muscle with the knee in extension can also produce pain due to patellar tendinosis. It must be kept in mind that the patient may present clinical hypersensitivity manifestations even in the absence of any injury identifiable by ultrasound(9).
[[{"fid":"5116","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"1":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Diagnostic methods
Ultrasound (US) and magnetic resonance imaging (MRI) are the most common techniques used to visualize the structure of the patellar tendon. Ultrasound presents a sensitivity of 58% and a specificity of 94% in application to patellar tendinopathy, with similar performance in the case of MRI (78% and 86%, respectively)(1,10). However, there is some controversy regarding the use of these imaging tests for the diagnosis of tendon lesions, since it has been seen that the correlation between pain and the structural alterations in tendinopathy is not linear(11). Furthermore, it is not clear whether the structural anomalies seen in the images are predictive of future symptoms or whether they are simply a normal physiological response to specific sports demands that do not indicate an increased risk of future symptoms. In 2016, McAuliffe et al.(12) concluded that structural ultrasound changes are associated to an up to 5-fold increase in the risk of developing tendinopathy, but that other factors are moreover required to trigger the clinical manifestations.
[[{"fid":"5117","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"2":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"2"}}]]
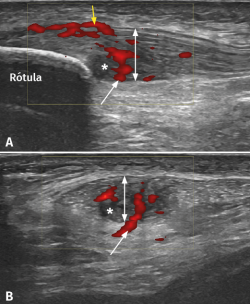
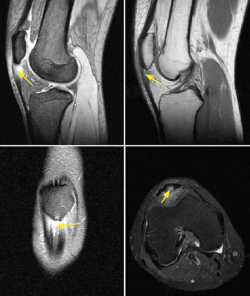
It has been demonstrated that both colour Doppler ultrasound (CD-US) (Figure 2) and MRI (Figure 3) are useful tools for confirming the diagnosis and can orientate treatment(10). Over the last two decades, ultrasound tissue characterization (UTC) has been developed with the purpose of obtaining even more information than conventional ultrasound. Indeed, the technique has become so important that some authors consider that UTC could be the most important development in medical US imaging since the introduction of Doppler ultrasound(13). Ultrasound tissue characterization is an imaging technique specifically designed for application to tendons. It is based on a colour scale that allows us to determine the degree of elasticity of the tendon tissue, and is able to measure small changes in tendon structure (e.g., as in evaluating the presence of tissue degeneration or fibrosis) - allowing us to establish an early diagnosis that can limit chronification of the process. The technique also has therapeutic applications as a tool for monitoring and guiding ongoing treatments, even after surgical repair, or for measuring the time for returning to physical activity (particularly in top athletes)(14,15).
[[{"fid":"5118","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"3":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"3"}}]]
Classification
A number of classifications can be found in the current literature. As a simplification, and to facilitate understanding, the existing tools can be divided into clinical- and imaging-based (using US and MRI) classifications. Some authors advocate classifying patellar tendinosis according to the Victorian Institute of Sport Assessment – Patella (VISA-P) score(16). This functional evaluation and monitoring scale will be explained in the section corresponding to functional assessment scales.
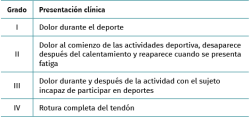
Classification of Blazina
Introduced by Blazina et al.(17) in 1973, this classification provides a qualitative description of the clinical progression of a patellar tendon injury. The different phases are described in Table 1. Roels et al.(18) subsequently modified phase 4, which represents complete tendon rupture.
[[{"fid":"5119","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"4":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"4"}}]]
Classification according to the duration of symptoms
Other authors such as Kaux et al.(19) recommend the classification of patellar tendinopathy as follows:
- Acute: symptoms duration between 0-6 weeks of evolution.
- Subacute: symptoms duration between 6-12 weeks.
- Chronic: symptoms duration > 3 months of evolution.
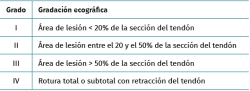
Classification according to lesion area
Gemignani et al.(20) classified patellar tendon lesions according to the percentage of damaged area. This is an ultrasound-based classification comprising four grades (Table 2).
[[{"fid":"5120","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"5":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"5"}}]]
Classification according to the magnitude of tendon rupture
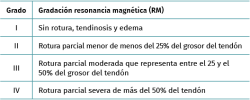
A recent study by Golman et al.(21) has classified patellar intratendinous lesions as corresponding to either partial or total rupture (Table 3). This classification is based on the MRI findings.
[[{"fid":"5121","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"6":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"6"}}]]
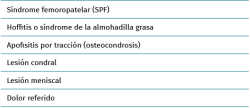
Differential diagnosis
[[{"fid":"5122","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"7":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"7"}}]]
Since the patellar tendon is an anatomical structure intimately related to the biomechanics of the knee, an analysis and study of the rest of the joint structures will be needed in order to establish a correct and detailed differential diagnosis (Table 4). In this regard, patellar tendinosis must be differentiated from:
Femoropatellar syndrome (FPS)
This syndrome is the most common cause of anterior knee pain(1). The condition is triggered by an alteration of patellar tracking within the trochlear sulcus, that can be influenced by a number of factors. The anatomical factors include trochlear width, inclination or patellar tilt. Biomechanical factors of the lower extremities also exert an influence, such as the femoral anteversion angle, measurement of the Q angle, genu valgus, recurvatum, tibia vara or foot pronation, among others. Mention also must be made of the muscular factors, such as weakness of the abductor and external rotator muscles of the hip, as well as of the knee extensor muscles. Lastly, a lack of elasticity of the flexor muscles of the hip and flexion-extension muscles of the knee also exert an influence (22). Seventy percent of all patients over 40 years of age with femoropatellar pain present a variable degree of osteoarthrosis of the joint(23), and this also may be concomitant to patellar tendinopathy. Clinically, the patient suffers mechanical pain associated to crepitation and variable limitation of daily living and sports activities. The diagnosis is established from the physical examination, and complementary confirmation tests are usually not necessary(24).
Fat pad syndrome
Fat pad syndrome is caused by impingement of the infrapatellar adipose tissue or Hoffa's fat pad on the anterior surface of the femur or tibia. The clinical manifestations are similar to those of FPS, and the disorder is more frequent in women between 30-40 years of age that perform repeated jumping exercises. The syndrome manifests as anterior knee pain that increases especially on walking up and down stairs, and may be associated to risk factors for this disorder (femoropatellar dysplasia, knee laxity and/or genu recurvatum(25). The diagnosis is based on the clinical and MRI findings(26). In the early 20th century, the orthopedic surgeon Albert Hoffa(27) described a diagnostic test that may be of interest: with the patient in supine decubitus and from a position of 90° flexion of the knee, we palpate the anterolateral part of the knee and, if pain manifests in the last 10° of extension, the sign is considered to indicate disease suggestive of inflammation of the infrapatellar fat pad.
Traction apophysitis
This disorder is generally found in pediatric patients. In relation to the insertions of the patellar tendon, we can find the following conditions: Osgood-Schlatter disease (in which the anterior tibial tuberosity [ATT] is affected) and Sinding-Larsen-Johansson syndrome (in which the lower pole of the patella is affected)(28). Osgood-Schlatter disease occurs as a result of repeated traction of the patellar tendon upon the ATT. It typically manifests during the peak growth period between approximately 8-13 years of age in girls and 10-15 years of age in boys, especially if the patient participates in sports that involve repeated jumping or continuous running(29). The diagnosis is established from the case history and physical examination. No complementary imaging tests are generally needed, though the presence of alarm symptoms such as nocturnal pain or a history of trauma would justify their use, and in this regard ultrasound affords very valuable information and is moreover noninvasive(30). On the other hand, the appearance of this disease condition in adults is related to direct trauma to the ATT(30).
Sinding-Larsen-Johansson syndrome shares clinical, diagnostic and therapeutic characteristics with Osgood-Schlatter disease, though in the former case the affected zone is the lower pole of the patella(31).
Chondral and/or meniscal lesions
Certain intraarticular injuries can cause pain similar to that of patellar tendinopathy, such as femoropatellar chondral lesions or anterior horn meniscal rupture. Radiographic joint cartilage modifications have been found in 4-10% of all patients between 15-24 years of age - a figure that reaches 80% in individuals over 55 years of age. Likewise, two out of every three knee arthroscopies evidence pathological chondral changes(28,32). Chondral lesions are clinically characterized by pain, effusion and mechanical symptoms. The pain behaves differently depending on the location of the lesion, and is more common when kneeling down, in maximum knee flexion positions, or on walking up stairs in patellar involvement, while in the case of femoral lesions the pain worsens with impact-generating activities. The diagnosis requires a full radiographic study, including axial views of the patella, and an MRI scan. A case series(33) study has described the appearance of lateral meniscus lesions and femoropatellar joint chondropathy, as well as Hoffa's fat pad disorders and synovial hypertrophy, in patients with chronic patellar tendinopathy.
Referred pain
A number of disorders can produce referred anterior knee pain without actual knee disease. For this reason, the physical examination of patellar tendinopathy must include a physical examination of the hip, since disorders such as adult coxarthrosis(34), Cam morphology femoroacetabular impingement, Perthes disease or proximal femoral epiphysiolysis in pediatric patients(35) can manifest as knee pain.
Functional assessment scales
Functional assessment scales are essential for ensuring a complete first diagnostic appraisal, since they include objective and subjective measurements that allow us to assess the patient course over time following therapeutic intervention.
Such scales examine objective parameters such as general health, pain and range of joint motion, among others, and also contribute subjective information such as patient satisfaction and expectations before and after treatment.
In order to perform a correct evaluation based on validated questionnaires, it is advisable to use at least one global health assessment scale, a pre-/post-injury physical activity score, and two scales specific of the disease condition requiring treatment(36).
Generic questionnaires for assessing health condition
The Short Form-36 (SF-36) offers a general perspective of the patient health condition and allows us to calculate the health-related quality of life profile. This tool consists of 36 multiple response questions that explore 8 different health dimensions (physical function, limitation due to physical problems, bodily pain, social function or role, mental health, limitation due to emotional problems, vitality, energy or fatigue, and general health perception), allowing joint assessment or the assessment of each concrete domain independently. The scores of each of the 8 dimensions of the SF-36 range between 0-100, where 100 indicates optimum health and 0 indicates very poor health. The responses assess the patient health condition of the previous month, and a second version has been developed that assesses the previous week. One of the inconveniences of this instrument is complexity in calculating the statistical result(37), though the questionnaire allows us to detect variations in health condition in multiple clinical disorders, and is the most widely used global health measure in orthopedic surgery and traumatology research(38). The SF-36 has a validated version translated into Spanish, which further facilitates its administration in our setting(39,40).
The Short Form-12 (SF-12) is the short (12 questions) version of the SF-36. It also allows calculation of the global health condition of the patient, and its main advantage is that it takes less time for the patient to complete - thereby facilitating its application. However, it is less potent than the original extended version, and does not allow us to obtain measures of the different health dimensions independently(36,40).
The Nottingham Health Profile is a questionnaire consisting of 38 yes/no questions. It is therefore easy for the patient to complete and is easy to analyse, since the result is a single overall score, which facilitates statistical use. The tool moreover has a second part comprising 7 questions referred to patient daily life(41). Its disadvantage in relation to the SF-36 is that it only assesses health/disease and does not allow us to study each domain independently. It has been used particularly in patients with osteoarthrosis of the lower extremities(36).
The EuroQoL was designed to complement other forms of measuring quality of life, and was specifically developed to generate a cardinal health index, which affords considerable potential for use in patient evaluation(42). The first part of the EuroQoL consists of 15 questions with three possible answers that explore mobility, personal care, daily activities, pain and depression, while the second part consists of a visual analogue scale for the assessment of patient global health perception(38). There is a validated version translated into Spanish, which facilitates its use in our setting(43).
Specific questionnaires for assessing knee disease and patellar tendinopathy
A range of functional assessment scales are available, specifically designed for application to knee function and pain. Considering that the symptoms of patellar tendinopathy are difficult to quantify, the current recommendation is to use two different subjective scales together with an objective assessment in the physical examination based on the pain provocation test(7).
The Victorian Institute of Sports Assessment for Patellar Tendinopathy (VISA-P) is the most widely used subjective scale for assessing patellar tendinopathy(16). This disease-specific clinical scale has been validated for patellar tendinopathy and contributes to its functional assessment(44). The VISA-P allows clinical classification based on the severity of symptoms, functional capacity and sports capacity, and helps both the healthcare team and the patient to quantify progress. In addition, it allows the early detection of any worsening of the symptoms. This tool consists of 8 items with a score ranging from 0-100 points. Optimum condition is represented by a score of 100. The validated version in Spanish of the VISA-P can be consulted at: https://www.jospt.org/doi/pdf/10.2519/jospt.2011.3613(45,46).
The visual analogue scale (VAS) is used to measure pain sensation as reported by the patient. This is a subjective, unidimensional and sensitive instrument that estimates pain intensity in disease conditions(44,47). Considered independently, these measurements are valid and reliable in application to many clinical settings - including the rehabilitation of patients with patellar tendinopathy(46,48). The VAS measures patient pain at the start and during rehabilitation, and offers precise evaluations of the intensity of pain and of variations in pain(44).
The combined administration of the VAS and of VISA-P is recommended, since both instruments are widely used in the rehabilitation of patients with patellar tendinopathy.
The other scales that have been proposed in the literature to complement the assessment of patellar tendinopathy are the Tegner activity scale, the International Knee Documentation Committee Knee Form (IKDC), the Kujala scale and the Knee Society Score (KSS).
The Tegner activity scale(49) is a subjective satisfaction score in which the patient rates his or her personal perception of general function of the operated knee. The activity level is scored from 0-10, where 10 is perfect (0 = disability; 1-4 = no physical activity, but able to work; 5-7 = leisure physical activity; 7-10 = competition physical activity). The scale arbitrarily groups sports activities into different levels without considering the frequency of such activities. Although the Tegner scale has not been statistically validated for use in Spanish and for reliability, it remains widely employed as a complementary assessment test(50).
The International Knee Documentation Committee Knee Form (IKDC) was developed in 1987, and one of its main objectives was the administration of a simple questionnaire that is easy to use and which can be employed to evaluate different disorders of the knee, including ligamentous, meniscal, patellofemoral and osteoarthrosis lesions. In addition, it allows the comparison of different groups with different diagnoses(51,52). The IKDC combines symptoms and signs. Each category is globally classified as A (normal), B (near normal), C (abnormal) or D (severely abnormal). The final evaluation of A, B, C or D is determined by the poorest score. This method comprises a subjective part of 18 questions that take into account the symptoms, sports activities and function. The scores are added and transformed into a scale from 0-100. The clinical evaluation part of the IKDC is divided into two sections: the first documents range of motion, the position of the patella, alignment of the knee and joint laxity. The second section in turn is divided into 7 groups (inflammation, limitation of passive motion, ligament assessment, compartmental findings, morbidity of the graft donor site, radiographic findings and functional test). The final result is determined by the lowest result of the group, in theory because the knee must be normal in order to achieve a perfect score. The IKDC has been validated for a range of conditions of the knee, including ligament, meniscal and joint cartilage injuries(53,54,55). It has also been standardized for different ages and genders(56).
The Kujala scale assesses pain and function in patients with patellofemoral joint disorders(57). It consists of 13 questions, each with 3 to 5 possible answers, scored from 0-5 or from 0-10, depending on the question. The lowest possible total score is 0 and corresponds to patients in poorer health functional condition. The highest possible total score is 100 and corresponds to patients with no alterations and who are in optimum conditions. This instrument has been validated in its Spanish version(58) and can be consulted at: http://www.scielo.org.co/pdf/cesm/v31n1/0120-8705-cesm-31-01-00047.pdf.
The Knee Society Score (KSS) has been developed by the American Knee Society. The Knee Society Clinical Rating System has evolved over time: the original version was modified by Insall(59), and this was followed by further changes to add new aspects and to simplify the tool, though preserving its integrity over time(60). At present, this is a scale where both the patient and the surgeon participate in the evaluation. It consists of a first knee score from 0-100 that evaluates pain, stability and range of motion (where 0 is the poorest score and 100 the best score), and a second score corresponding to knee function, with the same 0-100 scoring system. The surgeon completes the objective knee score, which includes a VAS score of pain on walking over a levelled surface, slopes or stairs, and also an evaluation of alignment, stability of the ligaments and the range of motion of the joint. Posteriorly, the patients record their degree of satisfaction, functional activities and expectations. This tool may present some interobserver variation. At present, it is the internationally most widely used assessment scale in knee replacement surgery(36), and has been validated in its Spanish version(61); it can be consulted at: https://link.springer.com/article/10.1007/s00167-013-2412-4.
Conclusions
Diagnostic approach
In patients with anterior knee pain, the medical history and physical examination suffice to establish the diagnosis. It is advisable to include a pain provocation test in the physical examination(8), consider differential diagnoses, and complement the study with diagnostic tests such as ultrasound, which allows us to confirm the diagnosis and classify the tendinopathy. Magnetic resonance imaging is indicated if the patient symptoms persist and ultrasound is unable to identify relevant findings.
Classification
Of the different proposed classifications, the clinical classification of Blazina is recommended, complemented by ultrasound-based classifications in view of their similar performance and lesser cost, and secondarily with MRI-based instruments. Both offer detailed information about the condition of the injury and its clinical course.
Assessment scales
The use of a global health assessment scale (SF-36), a pre-/post-lesion physical activity scale, and two specific knee functional scales (VISA-P and KSS) is advised.