Introduction
Tibiotarsal osteoarthrosis is the most frequent presentation of osteoarthrosis within the degenerative disorders of the ankle, and is less often associated to involvement of the subtalar joints. Whether combined or isolated, each of these conditions require specific treatment(1,2). In this respect, subtalar arthrodesis or fixation seeks to achieve solid fusion of the joint in order to eliminate pain and improve function. The most common indication of arthrodesis is painful posttraumatic subtalar osteoarthrosis following fractures of the calcaneus or talus. The indications can be expanded to primary subtalar osteoarthrosis, osteoarthritis following infection, flatfoot osteoarthrosis and other deformities(1,2).
Since the first subtalar arthrodesis procedure in 1912(3), adopting an open lateral and posterior approach, the technique has evolved greatly towards the current arthroscopic fixation techniques(4-22), with Tasto having been the first to describe the arthroscopic procedure(4). The growing interest in arthroscopic techniques is explained by the known benefits they afford in application to other joints: less surgical aggression, improved visualization and access to the structures, and a lesser incidence of complications that allows faster patient recovery. At present, and on the basis of the literature, it seems that most surgeons prefer the arthroscopic technique adopting a posterior approach(7,8,9,10,11).
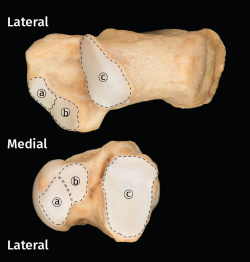
When arthrodesis is performed concomitantly (tibiotalar and subtalar), placing the patient in supine decubitus facilitates the operation. Cleaning and curettage of the subtalar joint (STJ) can be made in this position through two lateral portals in the tarsal sinus. In addition, the use of these lateral portals implies a lesser risk of iatrogenic damage to the surrounding neurovascular structures(23). For improved understanding, it is necessary to clarify that the STJ, comprising the subtalar joint surfaces of the calcaneus and talus, is described as being anatomically composed of three joint surfaces: anterior (AAS), medial (MAS) and posterior (PAS). However, in many cases the cartilage between the anterior and medial surfaces is continuous (Figure 1)(24).
[[{"fid":"5095","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"1":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
Our working hypothesis is that the denuded surface obtained through curettage of the PAS is the same through both the posterior and the lateral arthroscopic portals. The present study describes the results obtained in relation to percentage denudation of the STJ in human cadaver samples using either the posterior or the lateral arthroscopic portals, in confirmation of the established working hypothesis.
Methods
A descriptive observational study was made involving 12 ankle pieces corresponding to 6 human cadaver specimens, including the complete ankle joint in segments extending from the distal half of the tibia and fibula to the complete foot. It was checked that the specimens had no structural alterations capable of affecting the study. In this regard, one specimen with osteosynthesis material due to fracture had to be replaced. These anatomical pieces were prepared and preserved according to the method of Thiel(25), which allows greater cadaveric joint motion more consistent with that of the original joints. Both genders were equally represented (1:1 proportion), and the mean age was 57 years (range 45-70). Six specimens were assigned to the arthrodesis technique using lateral portals and the other 6 were assigned to the use of posterior portals. The same surgeon, specialized in foot and ankle surgery, performed curettage of the joint surfaces through the usual arthroscopy portals, both lateral and posterior.
Posterior portals technique in prone decubitus
Posterior, posterolateral (PLP) and posteromedial (PMP) portals were prepared following the technique described by van Dijk(22,26). A 5-mm incision was made lateral to the Achilles tendon. The subcutaneous layer was dissected using mosquito forceps, following by placement of the arthroscope with 30° angulation optics in the direction of the subtalar space. The accessory portal was placed medial to the Achilles tendon.
A 30° and 4.0 mm arthroscope (Arthrex, Naples, FL, USA) was used with a hydraulic pressure pump at 40 mm.
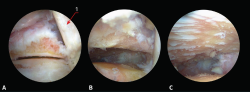
[[{"fid":"5096","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"2":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"2"}}]]
Synovectomy was performed using a 4-mm resection synoviotome (Arthrex, Naples, FL, USA). Soft tissue debridement was carried out until the subtalar joint space was located (Figure 2A). The tendon of the flexor hallucis longus muscle served as medial reference.
Following synovectomy and cleaning of the fibrous tissue, the posterior joint surface of the talus and calcaneus was visualized (Figure 2B).
We completed joint debridement and denudation of the cartilage with curettes, scoops and abrasion synoviotomes (Figure 2C), avoiding the creation of large spaces and using the portal exchange manoeuvre.
Lateral portals (tarsal sinus) technique in supine decubitus
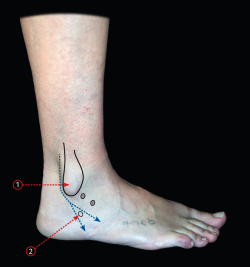
Two lateral portals were prepared, and the technique was performed as described(4). The lateral malleolus and tarsal sinus were used as anatomical references (Figure 3). A 5-mm incision was made 3 mm ahead of the external malleolus and behind the tarsal sinus. The subcutaneous layer was dissected using mosquito forceps, following by placement of the arthroscope with 30° optics obliquely in the direction of the subtalar space. With the arthroscope resting on the bone, the accessory portal was prepared under direct control (Figure 4A).
[[{"fid":"5097","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"3":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"3"}}]]
We used a 30° and 4.0 mm arthroscope with a hydraulic pressure pump at 40 mm.
Synovectomy was performed using a 4-mm resection synoviotome.
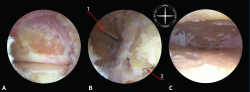
Following synovectomy and cleaning of the fibrous tissue, the cervical ligament of the tarsal sinus and the more lateral zone of the MAS corresponding to both the talus and the calcaneus were visualized (Figure 4B). If these ligaments are resected, the more medial zone of the SAM can be seen, though such resection is not indicated in clinical practice.
[[{"fid":"5098","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"4":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"4"}}]]
Joint cleaning was made with curved curettes and abrasion synoviotomes (Figure 4C), avoiding the creation of large spaces and using the portal exchange manoeuvre.
Quantification of the denuded surface technique
After completing debridement, each specimen was subjected to anatomical disarticulation, exposing the surfaces of the talus and calcaneus. The anatomical areas of the STJ were considered in the exposure (Figure 1)(27): PAS, MAS and AAS, correlating them to the areas that could be accessed with each of the surgical techniques employed. Digital photographs of the surfaces were obtained, and calculation was made of the denuded areas with each of the two techniques, using Image-J image analysing software (Wayne Rasband, National Institutes of Health, Bethesda, MD, USA), in concordance with common practice in studies of this kind(28,29).
Then, measurements were made of the total denuded surface area corresponding to both the talus and the calcaneus; the denuded area working from the PLP and PMP; and the combined area of these two working areas. The same calculations were made in the other 6 specimens in which the lateral portals technique was used. The measurements of the working area were correlated to the total area of the surface of the corresponding joint facet, expressed as a percentage. The Kruskal-Wallis test for the study of variables with a non-normal distribution was used to assess the influence of surface curettage. Statistical significance was considered for p ≤ 0.02.
Results
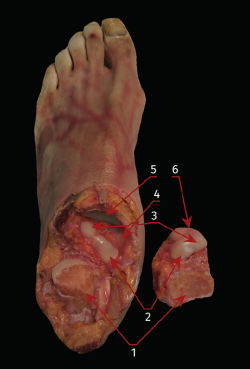
The posterior arthroscopic portals allowed an average surface exposure of 83.6% (range: 73.9-93.5%) of the PAS of the calcaneus and of 93.7% (range: 90.3-95.6%) of the PAS of the talus. However, percentage denudation of the MAS of both the talus and the calcaneus was practically negligible (Figure 5).
[[{"fid":"5099","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"5":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"5"}}]]
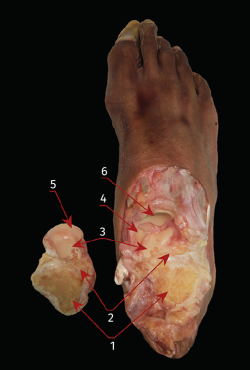
The lateral arthroscopic portals in turn allowed an average surface exposure of 88.8% (range: 79.9-91%) of the PAS of the calcaneus and of 81.2% (range: 71.8-92.3%) of the corresponding surface of the talus. Mean percentage denudation of the MAS was 84.6% (range: 74.9-92.8%) of the total joint surface of the calcaneus and of 83.6% (range: 70-92.8%) of the corresponding surface of the talus - though only in the more lateral zones (Figure 6).
[[{"fid":"5100","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"6":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"6"}}]]
The Kruskal-Wallis test evidenced no significant differences between the two types of approach in relation to the denuded surface. Comparison of the MAS following curettage showed significant differences in favour of the posterior portals (p = 0.02).
Discussion
The results of the present study show that it is possible to denude a similar joint surface of the PAS of both the calcaneus and the talus, using both the posterior and the lateral arthroscopic portals. However, access to the AAS is difficult if not impossible. It also seems difficult to denude the joint areas of the MAS through the posterior portals. In contrast, denudation of over 80% is possible using the lateral technique, but only in the most lateral zone. This could be the explanation for the higher pseudoarthrosis rate described in operated patients when only posterior portals are used, as well as for the longer consolidation time observed with this posterior technique(30,31).
The main contribution of the present study is that it involves a comparative analysis of the two techniques, while other articles are limited to examining one technique or the other(30,31). In their study of 10 specimens using posterior portals, Mouilhade et al.(18) were able to curettage an average of 97.5% of the same posterior joint surfaces, though undoubtedly at the expense of having to perform larger resections; as a result of this, the relief produced by the posteromedial process of the talus impeded adequate coaptation of the prepared surfaces in 8 of the 10 specimens. In our series, we were careful in avoiding such important resections that should not occur in clinical practice, even if the outcome is a lesser percentage of denuded surface. Nevertheless, percentage denudation was always over 60%, which is regarded in the literature as the minimum surface for guaranteeing adequate consolidation(23,32). Similar limitations were found by Lintz et al.(23), who in their case studied 30 cadaver specimens through lateral portals. These authors recorded a percentage preparation of 91.2% in the calcaneus and of 93.9% in the talus, though they likewise described limitations in extrapolating the results to clinical practice, due to the difficulty of finding the limits of debridement of the tarsal sinus and avoiding damage to the peroneal tendons.
The AAS could not be accessed through either of the two techniques. As has been reported, another two accessory portals would be needed for this(31). Access to the medial zones of the MAS also requires the use of accessory medial portals, as commented in the literature(31,). However, this implies a potential increase in the risk of causing neurovascular damage(15,18,28). If it is considered necessary to increase the percentage of denuded surface, we can combine the use of lateral and posterior portals(31), or an accessory portal(8,34).
As limitations of this study, mention should be made of the inherent nature of its design, involving samples from cadavers, and the limited number of specimens involved. Another limitation of studies of this kind is the fact that although the results obtained provide good guidance for surgical practice, no correlation is established, and consequently the data must be supported by the analysis of outcomes in operated patients.
Conclusions
In the studied sample, both the posterior and the lateral arthroscopic portals allowed over 80% denudation of the posterior joint surfaces of the talus and calcaneus. The lateral arthroscopic portals moreover allowed access and debridement of the MAS, with significant differences (p = 0.02). Only the lateral approaches to the tarsal sinus also allowed curettage of the lateral zone of the MAS. The AAS and the medial zone of the MAS could not be accessed through any of these portals.