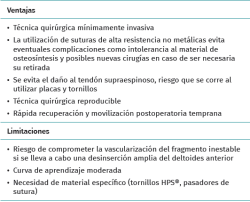
Introduction
The acromion originates from four separate ossification centres: the preacromion, the mesoacromion, the meta-acromion and the basiacromion, from anterior to posterior. Their fusion occurs between 18 and 25 years of age(1). The os acromiale is defined as the absence of fusion of any of the primary acromial ossification centres with the basal acromion (basiacromion)(2). It can be classified into three types according to the non-ossified segment located immediately anterior to the absence of fusion (preacromion, mesoacromion and meta-acromion), with mesoacromion being the most frequent presentation(3). The incidence of the condition is 1-15% in radiographic and anatomical studies(4). Affected patients usually present nonspecific symptoms. The manifestations may include pain (generally nocturnal), difficulty performing activities involving abduction above 90º, and weakness(5). It is important to establish a differential diagnosis and rule out other pain-causing disorders such as rotator cuff rupture, SLAP (Superior Labrum Anterior and Posterior) lesions or arthritic changes of the acromioclavicular (AC) joint(5).
Anterior acromial mobility, assessed through local palpation, is a clinical finding strongly suggestive of symptomatic os acromiale, and which in some cases may predispose to tendon rupture of the supra- or infraspinatus muscle(6,7).
[[{"fid":"5475","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"1":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"1"}}]]
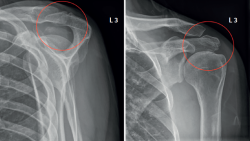
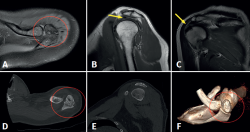
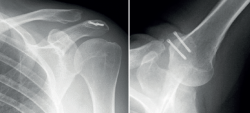
The basic imaging diagnostic explorations should include anteroposterior, axillary and scapular Y projection radiographs(Figure 1), with the axillary view being the most useful option in this regard(8). Magnetic resonance imaging (MRI) can identify additional disease conditions such as concomitant rotator cuff injury, for example(9). The presence of bone oedema in axial sections in fat-suppressed T2-weighted sequences is an expected sign in the MRI assessment of symptomatic os acromiale (Figure 2).
[[{"fid":"5476","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"2":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"2"}}]]
First line treatment should be non-surgical in all cases, based on the administration of nonsteroidal anti-inflammatory drugs or local corticosteroid infiltrations during a maximum period of 6 months(10). Nevertheless, surgery often proves necessary due to high refractoriness to conservative management(11,12).
A great variety of surgical techniques are available, with variable results(13,14,15,16,17,18).
The present technical note describes our preferred surgical procedure for mesoacromion type symptomatic os acromiale treatment.
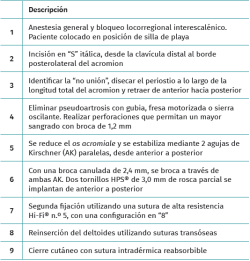
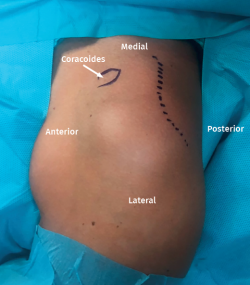
Surgical technique (Tables 1-3)
Under general anaesthesia and interscalene locoregional block, the patient is placed in deck chair position (Figure 3). Under conditions of asepsis and antisepsis, the surgical field is delimited and the anatomical references are marked (os acromiale, acromion, clavicle, AC joint and coracoid process), with planned incision (Figure 3).
[[{"fid":"5477","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"3":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"3"}}]]
An italic "S" skin incision of approximately 8 cm is made from the middle third of the clavicle to the posterolateral margin of the acromion, reaching the acromial periosteum (Figure 3).
[[{"fid":"5478","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"4":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"4"}}]]
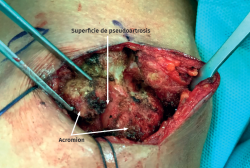
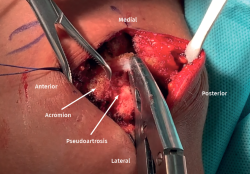
Mobility of the acromion is assessed by applying vertical pressure along its length. Once the non-fusion site of the os acromiale has been identified, the periosteum is dissected along the full length of the acromion and is retracted from anterior to posterior, exposing the margins of the non-fusion zone and allowing correct coverage at the end of the operation (Figure 4). The elevator is positioned between the os acromiale and the acromion to improve its exposure.
[[{"fid":"5479","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"5":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"5"}}]]
Full disinsertion of the deltoid muscle from the anterior margin of the acromion is not advised, in order to avoid damaging the terminal branches of the thoracoacromial artery.
[[{"fid":"5480","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"6":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"6"}}]]
If needed, release of the anterior deltoid should be the minimum required to allow manipulation of the mesoacromion and implant the osteosynthesis material.
[[{"fid":"5481","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"7":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"7"}}]]
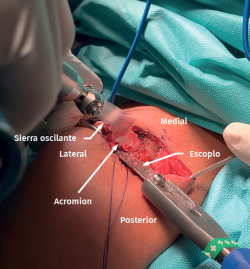
The pseudoarthrosis surface may be eliminated using rongeur type forceps, motorized drills or an oscillating saw (Figure 5). If a saw or drill is chosen, it is advisable to use a soft tissue protector with the aim of avoiding unintentional damage to the supraspinatus tendon (Figure 6). In order to favour consolidation of the mesoacromion, it is advisable to perforate orifices to allow increased local bleeding using a 1.2 mm drill.
[[{"fid":"5482","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"8":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"8"}}]]
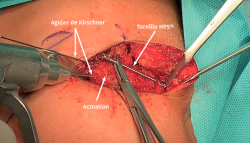
Following removal of the pseudoarthrosis, and after exposing the margins of the os acromiale, fixation is carried out. The os acromiale is reduced to its anatomical position and is provisionally kept fixed with reduction forceps. After confirming anatomical reduction, provisional stabilization is achieved with two parallel Kirschner wires (K-wires), perforating from the anterior margin of the exposed os acromiale to emerge from the posterior surface of the basiacromion, making sure that the K-wire is directed parallel to the acromial bone without invading the subacromial space.
[[{"fid":"5483","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"9":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"9"}}]]
At this point we determine the length of the screws needed for fixation, with the help of an additional K-wire to measure, or by superimposing the screw over the acromion (Figure 7).
[[{"fid":"5484","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"10":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"10"}}]]
With a 2.4 mm cannulated drill, we drill through the previously used two K-wires, and two partially threaded 3.0 mm HPS® screws (MedcomTech) are implanted from anterior to posterior in order to ensure the maximum compression possible.
[[{"fid":"5485","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"11":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"11"}}]]
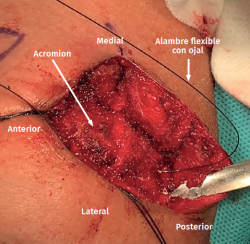
Once the cannulated screws have been positioned, the K-wires are removed and we apply a second fixation based on the tension band principle, using a high-resistance suture Hi-Fi® no. 5 (ConMed, FL, USA), tunnelled through the cannulated screws. Passing of the suture makes use of a flexible looped wire as transport mechanism (Figure 8).
[[{"fid":"5486","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"12":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"12"}}]]
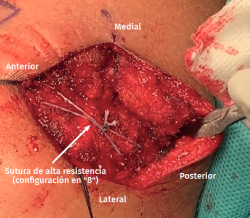
An "8" pattern is preferred, tightened with a sliding knot, manual tension and posterior 8-knot reinforcement, until no loss of tension is observed. This is a modification of the classical technique (19) based on the tension band principle with a 1-mm metal wire in a similar shroud knot pattern (Figure 9). The use of non-metal high-resistance sutures avoids possible complications such as intolerance of the osteosynthesis material, which could require further surgery for removal. Radioscopic control is carried out at the end of the procedure (Figure 10).
[[{"fid":"5487","view_mode":"default","fields":{"format":"default","alignment":""},"type":"media","field_deltas":{"13":{"format":"default","alignment":""}},"link_text":null,"attributes":{"class":"media-element file-default","data-delta":"13"}}]]
The periosteum is reinserted, securing full coverage of the construct. If disinsertion of part of the deltoid muscle is proved necessary, it is reinserted using transosseous sutures. The subcutaneous layer is then tightly sealed in place. For closing of the skin, intradermal suture with resorbable material is to be preferred.
Postoperative period
The patient is immobilized with a sling for two weeks. Passive joint balancing and pendular exercises are allowed from the immediate postoperative period and during the first four weeks. From week four, active mobilization can begin, together with strengthening exercises and activities of daily living. The return to sports activities is allowed after 6-8 weeks.
Discussion
There is no agreement as to which is the best option for the fixation of mesoacromion type unstable symptomatic os acromiale. Our preferred treatment strategy in such cases is the use of cannulated screws reinforced by a high-resistance suture tension band distributed in an "8" pattern, without added bone grafting and employing a transacromial medial to lateral surgical approach with minimum disinsertion of the deltoid muscle from the anterior margin of the acromion.
A number of techniques have been described for those cases in which conservative management fails: open or arthroscopic excision, acromioplasty or subacromial decompression, open reduction and internal fixation (ORIF).
Wright et al.(16) reported good outcomes with subacromial decompression in 13 patients after one year of follow-up. Campbell et al.(17) in turn performed arthroscopic excision of os acromiale in 31 shoulders. Complete pain relief was achieved in 20 of the shoulders, with improvement in 9. However, the appearance of deltoid dysfunction on resecting large fragments remains a cause of concern.
If ORIF of the symptomatic mesoacromion is decided to be performed, a number of options are available(11,18). The best results were recorded with the use of K-wires or compression cannulated screws, usually combined with a tension band (metallic in most cases)(20,21,22).
In a descriptive series of 15 cases of os acromiale published by Warner et al.(20), the patients were subjected to three surgical techniques: pre- and mesoacromion exeresis; ORIF with K-wire and cerclage; and ORIF with cannulated screws, cerclage and iliac crest autologous bone grafting. The best clinical outcomes were obtained with the consolidation of os acromiale and exeresis of the preacromion - the consolidation index being greater in the group subjected to osteosynthesis with screws, cerclage and grafting.
Similar results were reported by Peckett et al.(21), achieving consolidation of os acromiale within an average of four months in 25 out of 26 patients (96%) treated with tension bands and K-wires or cannulated screws. In the same way as the previous authors, Boehm et al.(22) recorded successful outcomes in 15 out of 22 patients (68%) subjected to fusion of os acromiale with isolated tension bands over a mean follow-up of 41 months.
A factor that may also favour successful ORIF is the use of autologous bone grafts(20,23), though this does not seem mandatory for achieving correct consolidation, provided stable fixation with acceptable compression is secured, as evidenced by the results published by Atoun et al.(13). These authors recorded radiographic consolidation in 6 out of 8 patients treated via arthroscopy with resorbable cannulated screws.
The vascularization of the unstable fragment would also play an important role in defining the outcome of osteosynthesis. It is believed that preserving the insertion of the deltoid muscle anterior to the os acromiale fragment (as recommended in the description of our surgical technique) would help preserve the acromial branch of the thoracoacromial artery. This, associated to fixation with cannulated screws and a tension band, appears to increase the percentage of consolidation. In this regard, Hertel et al.(19) documented a variable mesoacromion consolidation rate that appeared to depend on the surgical approach used. Fusion occurred in 43% of their patients subjected to a trans-deltoid approach versus in 88% of the cases when a transacromial approach was used.
A significant problem is the high incidence of intolerance and extraction of the implanted material following ORIF - a circumstance that may lessen the favourable opinion of the patient regarding the outcome of surgery. These figures are much higher with the combination of K-wires and cerclage than when using the cannulated screw and tension band technique, as reported by Warner et al., Hertel et al. and Peckett et al., with percentages of between 86-100%(15,19,20).
This high implant intolerance rate reflects the potential advantage of a fixation method with a lower profile, such as the combination of a tension band using high-resistance sutures together with cannulated screws(14,24), as described in the present technical note. Such a combination would afford biomechanical resistance similar to that of stainless steel wire cerclage, according to the data published by Shui et al.(25) in a study in cadavers.
Our study shows that the fixation of symptomatic os acromiale using cannulated screws and tension bands with high-resistance sutures allows consolidation of the mesoacromion without the need for secondary procedures (material ablation), and without complications.
The optimum results recorded define this surgical technique as a reproducible alternative to be taken into account in infrequent cases of symptomatic os acromiale.